Skin Mole Mapping – Videodermatoscopy (Canfield D200 Evo)
High-resolution skin imaging to monitor moles and detect early signs of atypical or malignant changes.
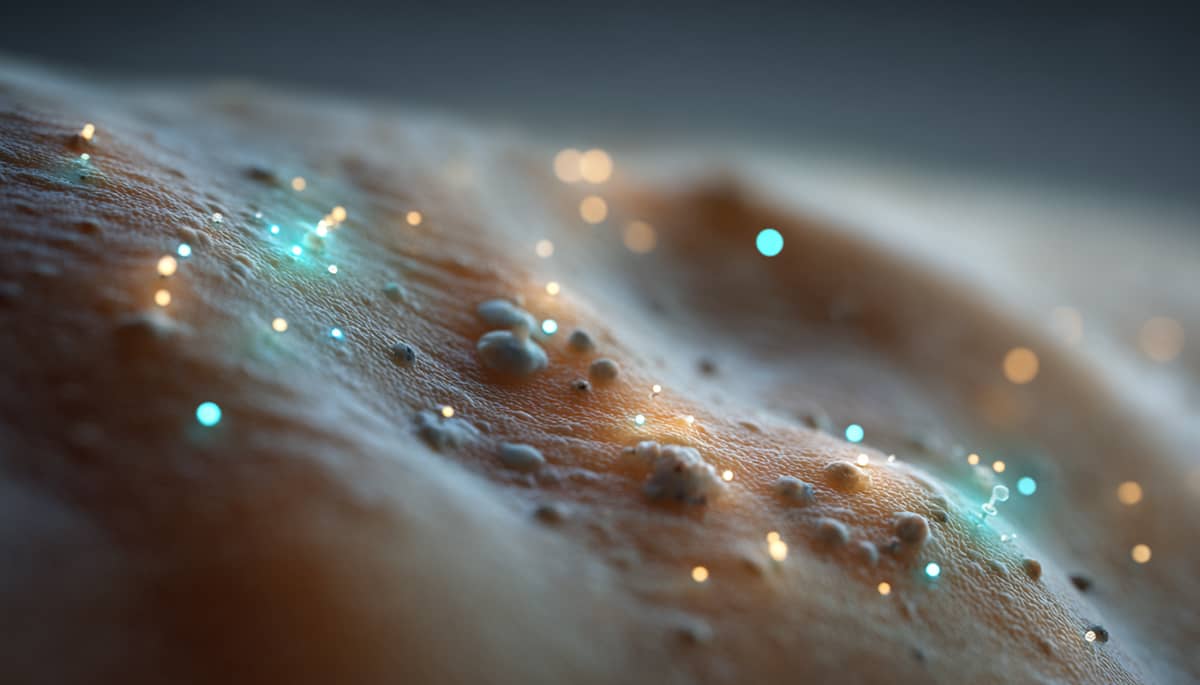
Table of contents
Basic data
The Skin Mole Mapping examination uses videodermatoscopy — a high-resolution imaging technique that allows detailed visualization and documentation of pigmented skin lesions. Using the Canfield D200 Evo system, this test enables dermatologists to analyze the structure, color distribution, and symmetry of moles and identify early features suggesting atypia or malignant transformation.
The examination is non-invasive, quick, and provides a digital baseline for long-term monitoring of existing lesions. It is an essential component of skin cancer prevention programs, especially for individuals with multiple moles, fair skin, or a family history of melanoma.
Category: Imaging
Level: Intermediate
Usefulness: High
Level
Intermediate
Usefulness
High
Early detection of skin cancer
Identifies early atypical or malignant transformations, enabling timely medical intervention and higher treatment success rates.
Precise long-term monitoring
Provides high-quality digital records for yearly comparisons, helping track subtle mole changes over time.
Non-invasive and safe
The procedure is painless and free of radiation, suitable for adults and children alike.
How it works
Imaging process
The clinician captures magnified, high-resolution images of moles across body regions using the Canfield D200 Evo system, which provides up to 200x magnification and standardized lighting for diagnostic consistency.
Digital documentation
All mole images are stored in a database, allowing precise comparison during future follow-up examinations to identify any new or evolving lesions.
Measures
Pigment structure and symmetry
Evaluation of color distribution, border regularity, and internal pigment network patterns.
Atypia indicators
Detection of dermatoscopic features that may suggest risk of malignant transformation.
Reliability
Repeatability
High reproducibility when performed under similar lighting and magnification conditions, enabling accurate longitudinal monitoring.
Diagnostic accuracy
When combined with expert dermatologic interpretation, sensitivity for melanoma detection exceeds 90%.
Limitations
Requires expert interpretation
Diagnostic accuracy depends on clinician experience and quality of image acquisition.
Limited to visible lesions
The method cannot assess subdermal or systemic conditions and only applies to surface-visible skin changes.
Frequency
Suggested cadence
Once per year for individuals with multiple moles or higher melanoma risk; every 6 months if new or atypical lesions appear, or as advised by a dermatologist.
Cost
Typical costs
Approximately €100–200 depending on the clinic and number of lesions examined.
Availability
Where available
Offered by dermatology and longevity clinics equipped with Canfield or Fotofinder videodermatoscopy systems.
Preparation
How to prepare
Avoid applying makeup, sunscreen, or body lotion to the areas to be examined. Ensure good skin hygiene and bring previous imaging reports if available.
Interpretation
No atypia
Indicates benign, symmetrical mole structures with no signs of malignancy. Annual follow-up is recommended.
Atypical features
Suggest the need for closer observation, shorter follow-up intervals, or biopsy if structural irregularities are observed.
Alternatives
Manual dermatoscopy
A simplified version using a handheld dermatoscope without digital recording — useful for single-lesion evaluation but lacks longitudinal tracking capability.
Total-body 3D skin imaging (Fotofinder ATBM)
An advanced full-body mapping system that provides 3D skin visualization and automated mole comparison over time.
FAQ
Is videodermatoscopy safe for frequent use?
Yes. The procedure is completely non-invasive, radiation-free, and suitable for regular annual or biannual monitoring.
Who should undergo mole mapping?
Anyone with numerous moles, fair skin, family history of melanoma, or high UV exposure should consider annual videodermatoscopic assessment.
Can this test detect all types of skin cancer?
It can identify suspicious pigmented lesions but cannot replace biopsy or histopathological confirmation when malignancy is suspected.